Abstract

Hydroxyurea (HU) is an important drug for sickle cell disease (SCD) that improves clinical outcome and survival. However, its pharmacokinetics (PK) and pharmacodynamics (PD) are highly variable. HU has an excellent oral bioavailability, with half-life of 2-4 hours and renal elimination. Two oral absorption phenotypes have been identified: slow phenotype with a peak concentration reached after 60 to 120 minutes and rapid phenotype with a peak at 15 to 30 minutes. These phenotypes seem to be linked to the maximal tolerated dose of hydroxyurea and could affect the response to HU.
The aim of this study was to explore the possible correlation between clinical and biological response to HU and PK and PD parameters.
This study was conducted at Hôpital Universitaire des Enfants Reine Fabiola (Brussels, Belgium) and included SCD children older than 7 years, regularly followed for more than 3 years. PK samples (salivary and plasmatic) were collected at 0, 30, 60 and 180 minutes after oral HU intake. Patients have been classified as good (GR) or poor responders (PR) to HU according to the absence of recurrence of acute chest syndrome on HU and the number of vaso-occlusive crisis (VOC) and hospitalization days on HU. Changes in biological parameters were assessed after 1 year on HU. Chi square test was used for the comparison between good and poor responders on HU. Paired T test was used to compare biological effect of HU for each oral absorption phenotype and ANOVA to compare PK profile among them.
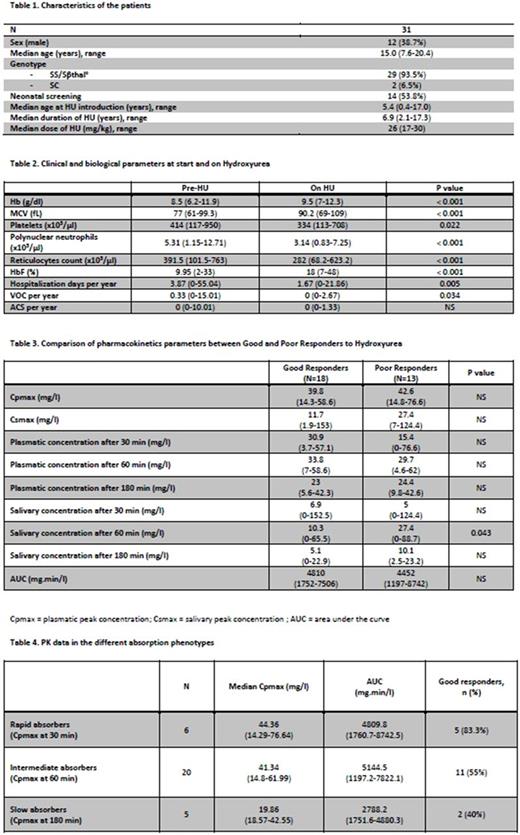
Thirty-one patients have been included in this study. The characteristics of the patients are detailed in the Table 1. On HU, a significant decrease of the number of VOC and hospitalization days was observed with an improvement of biological parameters (Table 2). The numbers of VOC and hospitalization days were significantly lower in girls compared to boys on HU (0.33 vs. 0, P=0.02 and 3.17 vs. 1.33, P = 0.02 respectively). However except for reticulocyte count, biological data, age, dose of HU or PK parameters were similar in both sexes.
Eighteen patients have been classified as GR (14 girls) and 13 as PR (5 girls). Their demographic characteristics and biological values (pre and on HU) were not significantly different, except a higher change of HbF level in GR compared to PR (+13% vs. +3.7% ; P=0.034). Girls had a non-significant trend to belong to the GR group (P = 0.059).
The median plasmatic peak concentration (Cpmax) was 42.25mg/l (Range: 14.8-62), the median salivary peak concentration (Csmax) was 19.54 mg/l (Range: 5.03-124.43) and the median AUC was 4650mg.min/l (Range: 1197-8742). AUC was similar in both sexes (4650mg.min/l vs. 4666mg.min/l; P=0.79). Except for salivary concentration at 60 minutes, all PK parameters were not significantly different between the GR and PR (Table 3). No significant correlation was found between peak concentration (Cmax) and demographic parameters.
We identified 3 absorption phenotypes with a Cpmax reached at 30, 60 and 180 minutes for rapid, intermediate and slow absorbers (Table 4). Biological changes on HU were similar among the 3 phenotypes, but did not reached statistical signification in slow absorbers (only 5 patients). 16/18 GR patients reach Cpmax at 30 and 60 minutes compared to 10/13 for PR (P=0.63). The AUC in the 3 absorption phenotypes was not significantly different (P=0.069). No correlation was found between salivary and plasmatic concentration at time-points studied.
In conclusion, no correlation between the absorption phenotype and the clinical response to HU could be found. No correlation was found between AUC, Cpmax and clinical response. Nevertheless our study has limitation due to the limited sample size. Salivary measurement did not provide reliable information and cannot be used instead of plasmatic samples. The gender is the only factor identified that can predict the biological response to HU (with a trend to a better clinical response in girls) despite similar AUC and PK parameters. This finding may reflect the better adherence to treatment in girls compared to boys.
The variability of the clinical response to HU remains to be elucidated.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal